Abstract
This
article uncovers the relevance to
practice of behavioural and social determinant models of HIV prevention
among
Yoruba women in Nigeria. Exploring what factors influence health
behaviour in
heterosexual relationships, the key question raised was whether the
women’s
experiences support the assumptions and prescriptions for action of
these two
dominant public health models. Eight focus group discussions and 39
in-depth
interviews were conducted, which involved 121 women and men who were
chosen
purposefully and through self-nomination technique. This study revealed
that
the women were very much constrained by social environments in
negotiating safe
sex, despite having at least a basic knowledge of HIV prevention.
Limiting
factors included the fear of relationship breakup, economic dependence,
violence, and the difficulties in justifying why they feel the need to
insist
on condom use, especially since initiating condom use is antithetical
to trust.
Furthermore, evidence suggested that improved access to income and
education
might be vital but it does not automatically constitute a direct means
of
empowering women to prevent HIV infection. The limitations of both
behavioural
and social determinants perspectives thus suggests the need for a
combination
prevention model, which focuses on how social, behavioural and
biomedical
factors overlap in shaping health outcomes.
Keywords
HIV/AIDS
prevention, Yoruba women, Nigeria, social
determinants model, behavioural model
Introduction
In
Nigeria, 88 per cent of women and 94 per cent of men
have heard about HIV/AIDS (National Population Commission [NPC] and ICF
Macro,
2009). Despite this awareness, this country has the second largest
population
of infected people globally and women remain mostly disadvantaged and
susceptible (United Nations General Assembly Special Session, 2010).
After decades
of seeking answers to HIV problems, the challenges are still daunting
mainly
because of a lack of clarity about how to address the needs of
different
populations. The global response remains hampered as policy makers,
experts,
and donors continue to hold different views of how to achieve effective
interventions. To understand why current interventions have failed to
deliver
effective outcomes among Yoruba women in Nigeria, I explored the
factors that
make them more vulnerable, and whether the solutions lie in the two
dominant
but seemingly contrasting perspectives that shape HIV policies and
strategies,
as underpinned by a behavioural model (BM) and a social determinants
model
(SDM).
On
philosophical and scientific grounds, proponents of
SDM hold that social inequalities cause and closely mirror health
inequalities
within and between countries (Gupta et al., 2008; Marmot et
al.,
2008). This model deploys a ‘functional’ meaning of health
and illness that
portrays health inequalities a consequence of social hierarchies that
follow a
social gradient. Deriving its philosophical influence from the
principles of
social justice (Commission on Social Determinants of Health [CSDH],
2008;
Ruger, 2004), SDM is consistent with the theory of justice according to
Rawlsian
‘liberal’ model, which supports the need for socioeconomic
and political
restructuring that allows more fairness in the distribution of life
opportunities (Rawls, 1971). Additionally, the origin of SDM can be
traced to
social epidemiology, which studies how social environments shape the
distribution of health and illnesses among populations (Berkman and
Kawachi,
2000).
My
assessments of SDM in this article centre
particularly on the influential final
report of the World Health Organization (WHO) Commission on Social
Determinants
of Health, which gathered a mass of evidence about how social and
structural
factors constitute health inequalities within and between countries
(CSDH,
2008). One of the main assumptions is that unequal access to power,
income,
resources, and services, has significant negative implications for
health
choices, behaviour, and outcomes. Accordingly, SDM prescribes global
health
reforms that take into account circumstances in which people are born,
grow,
live, work and age, and how such circumstances influence their health
outcomes
(Wilkinson and Marmot, 2003; CSDH, 2008).
Sub
Saharan Africa (SSA), in particular, remains
disproportionately affected considering the global inequalities in HIV
incidence. In 2011, this region accounted for 69% of the global
population of
people with HIV/AIDS, 70% of HIV related deaths, and 80% of all people
with
both tuberculosis and HIV (Joint United Nations Programme on HIV/AIDS
[UNAIDS],
2012). In terms of gender distributions, women and girls are still
mostly
affected, accounting for 58% of the infected in this region and bearing
the
greatest burden of care (UNAIDS, 2012). In spite of this challenge, the
global
responses to HIV/AIDS still foster inequalities, as many observers have
noted.
Lisk (2010) explained that although the burden of HIV/AIDS is
concentrated in
developing countries of the South, the current global health system
still
favour resource rich countries of the North, not only in terms of
access to
treatment and funding, but also in relation to decision-making
authority within
key global institutions.
Unlike
SDM, which focuses on how socioeconomic and
political environments shape health outcomes, BM focuses on how
individuals
make calculated decisions about their health behaviour. Significantly
influenced by Skinner’s work on operant conditioning (Skinner,
1938), BM
attempts to make predictions about observable human health behaviour,
which
could be rigorously examined through scientific investigations.
Although there
are different strands of BM, they all share assumptions that support
individual
level interventions drawing on the argument that: (1) health behaviour
is a
matter of rational choices; (2) it is predictable based on
peoples’ knowledge
of the consequences of their actions and the degree to which they value
health
(Rimer and Glanz, 2005; Rosenstocket al., 1994; Fishbein, 2000;
Fishbein, 2008; Prochaskaet al., 2008). Accordingly, HIV
policies shaped
by BM are often sympathetic to public health communications designed to
heighten
people’s perception of their vulnerability to infection, and to
those that
raise awareness about the severity of AIDS and benefits of risk
reducing
behaviour (Blumberg, 2000).
Both
SDM and BM have drawn criticisms. According to
critics, SDM lacks a clear functional definition, which can translate
to
rigorous evaluations of health programmes that follow the prescriptions
of the
model (Moulin, 2008; Kim et al., 2008; Argemiaet al.
2012;
Navarro, 2009; Stevens, 2009; Bambra, et al., 2010). In
support, some
writers have argued that it is inaccurate to consider poverty or
socioeconomic
inequality a direct driver of HIV/AIDS (Shelton et al., 2005;
Gillespie et
al., 2007). Likewise, critics of BM have argued that it is narrow,
mechanistic, and only responding to a fraction of populations’
health needs by
failing to take into account causal pathways to health that have their
roots in
social, economic, legal, and political structures (Blas et al.,
2008;
Amaroet al., 2001). To contribute to this debate, I explore in
this
article whether the participants’ behaviour, in preventing
HIV/AIDS, supports
the assumptions and prescriptions for action of both models.
Methods
A
qualitative approach was the most appropriate in
conducting this study (Rubin and Rubin, 2012) because key to my
objectives was
the need to elicit data that were capable of detailing people’s
experiences and
practices in relation to HIV prevention (Power, 1998).
Ethnographic
method was used to explore how the participants make meanings of their
everyday
life (Fetterman, 1998) in heterosexual relationships. A pilot was
conducted,
which shaped the main investigation process. The study was conducted among Yoruba people in Osun
state, Nigeria, and data were obtained through
focus group
discussions (FGDs) and in-depth interviews (IDIs) (Rubin and Rubin,
2012;
Stewart et al., 2007). On average, each FGD took one and half
hours,
while an IDI took one hour. The investigation process involved digital
voice
recording and note taking. Altogether, there were 121 women and men
participants (see table 1 below), who were recruited from their houses,
market
places, religious, community and health centres, an academic
institution,
public offices, private business centres,
and
farm areas.
Purposeful
sampling and self-nomination technique were
used in selecting the participants because these methods allowed an
ethical
investigation process and efficient access (Dane, 1990). Given
the
criticism that selection techniques in qualitative studies are prone to
bias
because of over reliance on purposeful sampling (Watters and Biernacki,
1989),
I introduced stratification to the sampling process by dividing the
participants into six respondent groups. These included low and high
socioeconomic status women, low and high socioeconomic status men, HIV
positive
people, and local HIV prevention workers. With a clear definition of
eligibility for participating in each group, this approach supported
eliciting
data from samples that were representative of adult populations in the
study
area, in terms of gender, HIV/AIDS experiences, and socioeconomic
classifications. Those identified as low socioeconomic status
participants had
little or no education, and a low income. The high socioeconomic status
participants included those with at least a university degree and a
relatively
high income. Ages in all the groups ranged from 20 to 71.
Those
identified as HIV positive were recruited from a
HIV treatment centre and a local HIV organization. The selection
process was
self-nomination, in which individuals indicated their willingness to
participate. For ethical reasons, the participants in this group were
not
contacted until after they had given informed consent to participate.
The
officials at the centres organized the consent process. They were
specifically
told not to make people feel pushed to participate in the study
(Economic and
Social Research Council [ESRC], 2012).
All
the participants shared two characteristics; they were
in long-term heterosexual relationships and had at least a basic
knowledge of
HIV prevention. Because this was a sensitive study, with the potential
to cause
the participants harm or offense (Lee, 1999), and because of the
challenges of
obtaining permissions from gatekeepers (ESRC, 2012), no persons below
the age
of 18 were included. By explaining to them in detail the nature of this
study
and my responsibility to protect their confidentiality, all the
participants
were supported to make informed decision whether to participate or not
(Wiles et
al., 2006). The FGDs was conducted in enclosed spaces, which the
participants and I considered safe and suitable. A minivan was used as
a mobile
interviewing space for the IDIs. This strategy allowed effective
logistics and
privacy. Data analysis involved translating most of the data from
Yoruba to
English. After examining the transcript and identifying themes, which
had
emerged from the data, NVivo 8 was used in coding and categorising the
data
under different themes (Welsh, 2002). A limitation of this study might
be its
reliance on data obtained through self-reports, given that individuals
often
have the tendency to misreport their true experiences in sexual
relationships
(Mongkuoet al., 2010).
Results
and Discussion
To
present a clearer analysis of whether the women’s
experiences support SDM and BM, it is appropriate to present the
results and
discussion together. The participants are identified by the groups they
belong
to protect confidentiality: low status woman (LSW), high status woman
(HSW),
low status man (LSM), high status man (HSM), HIV positive (HP) and HIV
prevention worker (HPW). The analysis is divided into two main themes,
which
are social determinants of HIV/AIDS and behavioural determinants of
HIV/AIDS.
Social
determinants of HIV/AIDS
This
section indicates various social factors that shape
the behaviour of Yoruba women in relation to HIV prevention. These
factors are
categorised into seven sub-themes, which are; permanence of
relationships, trust,
economic dependence, fear of violence, religion and gender roles,
culture of
silence about sex, and desire for fertility. These factors are
discussed below.
Permanence
of relationships:
Discussing their views and experiences about sex in a regular
heterosexual
relationship, all the respondents indicated that a breakup is the most
likely
consequence if a woman attempts to exercise a greater degree of control
over
her sex life. This is a hidden factor, which writers rarely discuss in
HIV
literature and yet is capable of constraining women’s ability to
prevent HIV
infection. Because people place so much value on permanence of
relationships in
this society, women are socially constrained either in terms of
exercising
control over their sex lives or in deciding to leave a relationship
they
consider harmful. Discussing her experience, a LSW said that, ‘I
have never
tried to make independent decisions about my sexual and reproductive
life.’ Her
reason was that, ‘I do not think it’s wise for me to push
my husband to other
women, people will blame me.’ To exercise such control, she
suggested that her
society would consider her actions opposite to cultural expectations
about
women’s gender roles, which include satisfying partner’s
sexual preferences.
Most of the low status women indicated that they shared this experience
when
they said that, ‘it is difficult to initiate or insist on condom
use’ with
their partners, even when they had doubts about partner’s sexual
fidelity.
Given
that most of the low status women were economically
dependent on their partners, I initially held the view that they were
actually
concerned about the economic consequences of relationship breakup
rather than
worried about breakup itself. To understand the significance of this
social factor,
I investigated how it affects the behaviour of the high status women.
Evidence
showed that they were constrained in a similar manner even though they
seemed
to be economically independent. To experience a breakup is a serious
concern
for all the women because of the social implications. A HSW stated,
‘the Bible
says divorce is a sin,’ and thus suggested that she would avoid
any actions
that could lead to this, including exercising control over her sex
life, which
is necessary for women to reduce their vulnerability to HIV infection.
Besides
religious factors, relationship breakups often attract undesirable
labelling in
this society, as another HSW said:
Even
as a university lecturer, I cannot say that I have
control over my sex life. You know people would scare you when they
say, “look
at that professor, she was left by her husband because she was
demanding gender
equality.” This is how people stigmatise divorced women in our
society.
Sharing
her experience, a HSW corroborated the earlier
comments. She had separated from her husband because, ‘he wanted
me to accept
his infidelity as something normal for men and was therefore exposing
me to HIV
infection.’ She explained that, ‘our relatives and friends
criticised and
mistreated me for taking this action.’ While justifying her
action, she said,
‘this is a very difficult path to take but we must make our
society accept that
women should not be compelled to stay in relationships that endanger
their
lives.’ Unable to do the same, another HSW stated that she knew
the danger of
unsafe sex. However, ‘there are many girls out there who are
ready to do
whatever men want, so why should I drive mine away’ by trying to
insist on
condom use. These women did not suggest to me that they feared
relationship
breakups more than the risks of HIV infection. However, their comments
illustrate that social values and traditions are capable of
constraining women
in their efforts to prevent HIV/AIDS. This evidence is consistent with
SDM by
suggesting that it is inaccurate to limit women’s sexual health
behaviour to a
rational choice perspective, as it is the case that social environments
often
play a major role in shaping their behaviour. Because of her limitation
in
exercising a greater degree of control over her sex life, a LSW said
that, ‘all
I can do is to trust that he would not bring any disease to me.’
Trust:
This emerged as another
key social factor that constrains the ability of Yoruba women to
undertake
risk-reducing behaviour. The social context in this society encourages
partners
in monogamous marital relationships to have shared expectations about
trust
unless there is concrete evidence of unfaithfulness. Such expectations,
however, have serious implications for HIV transmission and infection
in terms
of fostering false hope about individual’s vulnerability (Bowleg et
al.,
2000; Sobo, 1995). For example, A LSM said that, ‘I do not use
condoms if I
trust a woman.’ In addition, all the participants who were
identified as HIV
free expressed that they would normally expect their partners to
consider
unprotected sex with them a risk free practice. For that reason, most
of them
said that they would construe condom initiation by a long-term partner
as an
indication of concerns about their HIV status. However, unlike men,
onus is
usually on women to justify why they feel the need to avoid unprotected
sex.
The acceptable justification is to provide concrete evidence that
support
claims. Because it is difficult to obtain such evidence, women in this
society
are vulnerable to HIV infection, a HSW indicated:
No
matter how empowered we are as women, and how
skilfully we can negotiate, it is not easy to insist on condom use,
even when
we think we are at risk. From my own experience, I know that men are
more
likely to deny having affairs but they expect us to trust them.
A
LSW agreed to the previous comment by saying that, ‘I
am faithful to my partner but I do not know what he does outside, so
there is
nothing I can do.’ This finding indicates the limitations of the
ABC
(Abstinence, Being Faithful, Condomise) strategy as underpinned by BM
of HIV
prevention. According to critics, this strategy has failed to take into
account
underlying contextual factors outside individuals’ control that
make monogamous
women in marital relationships vulnerable to infection(Murphy et al.,
2006).Sharing her personal experience, a HP woman illustrated how
expectations
about trust in sexual relationships could increase women’s
vulnerability to
HIV/AIDS: ‘My husband kept his HIV status secret from me until
his death. I
only saw his treatment card after his death.’ This woman
indicated that she was
faithful to her partner. However, she was infected because of trust and
lack of
concrete evidence that HIV infection was imminent by having unprotected
sex
with him.
Supported
by findings from this study, literature has
shown that 81 percent of women in Nigeria would refuse sexual
relationships
with a partner known to have sexually transmittable infections (NPC and
ICF
Macro, 2009). This implies that encouraging partners in long-term
relationships
to test and disclose status can give women the real empowerment to
prevent HIV.
A LSW said that, ‘no matter what the consequences might be, if I
know that my
husband has HIV, I will insist that he uses condoms before having sex
with me.’
She added that, ‘if he refuses, I will never allow him to sleep
with me.’
Sharing a similar view, a HSW stated, ‘If I have compelling
evidence that my
husband has HIV, I will be very serious about keeping myself
safe.’ These
comments seem to support the assumptions of BM that people would
undertake
recommended behaviour if they understand the severity of a health
problem and
value health (Glanzet al., 2002). However, the problem is that
these
women also indicated that they were unlikely to insist on condom use
based on
suspicion alone. Thus, vulnerable individuals could be at risk for as
long as
they are unable to prove that their partners are exposing them to HIV
infection. The main point therefore is that conformity to social
expectations
can be a risk factor, especially regarding the issue of trust in sexual
relationships. This finding raises questions about whether HIV
prevention
programmes should support the culture of suspicion as part of the
strategy to
encourage women to anticipate risks. This would require extensive
research to
understand the wider implications for women’s wellbeing.
Economic
dependence:
Evidence also emerged that this factor was a concern shared by all the
low
status women, and possibly the most significant constraining factor. As
a LSW
indicated, an attempt to exercise control over her sex life could lead
to
abandonment, in which ‘my husband could ask me to pack out of our
house.’ While
reflecting on the possible economic implications, she said that,
‘I would not
be able to cope on my own,’ dealing with her financial needs and
those of her
children. George and Jaswal in a study of low income women in India (as
cited
in Gupta, 2002) have indicated that disadvantaged women are more likely
to be
worried about the economic implications of leaving a relationship that
they
consider harmful than the health risks of staying in such a
relationship.
Corroborating
this evidence, most of the men in this
study indicated that they would normally exploit their position as the
breadwinner to force their sexual preferences on their partners. While
they
concurred that, ‘decision making is men’s
prerogative’, they also considered
the sharing of power and control with women in sexual relationships
unacceptable. A HSM added, ‘No, my decisions would always
override her
decisions.’ Although economic empowerment might be crucial for
women to
exercise a greater degree of control over their sex lives,
investigations with
the high status women suggested that access to economic power does not
automatically constitute a direct means of empowering them to prevent
HIV/AIDS.
For example, a HSW said:
It
is difficult to insist on condom use but more
difficult to abstain from sex as a married woman. Although condom use
might be
the best mean to protect myself, this is only possible if my husband
agrees.
Supporting
the above comment which suggests that women
cannot be empowered unless men are involved, a HPW stated that,
‘100 percent of
our female clients said they could not insist on condom use when their
partners
refused.’ This finding raises caution about the assumptions of
SDM, which
suggests that improved access to power, income, resources, and
services, would
make a big difference to women’s health choices, behaviour, and
outcomes. It is
important that improved access to economic power is not mistaken as
empowerment. Instead, the focus should be on whether women are able to
use
their access to life opportunities to achieve substantive freedom and
control
over their lives (Sen, 2001), without the fear of consequences, such as
intimate partner violence, which is another major constraining factor.
Fear
of violence:
Violence against women is a violation of their human rights, which has
serious implications
for their health outcomes. For most of the women participants, being
resolute
about condom use in their sexual relationships is more likely to
attract
violence from partners. A LSW who had experienced such violence stated
that,
‘there would be trouble again if I tell my husband that I will
not allow him to
have sex with me unless he uses condoms.’ She recalled and said
that, ‘my
husband did not beat me because I asked him if he was having
affairs,’ but he
turned violent because, ‘I refused to have sex with him to
protect myself from
HIV.’ This woman indicated that her experience with violence is
such a strong
force that has been constraining her ability to make the right health
choices.
This finding weakens the rational choice assumptions of BM. Similarly,
a HSW in
her account indicated that there is a strong connection between gender
violence
and women’s inability to exercise control over their lives:
My
husband had abused me physically and this experience
has affected my political career. He did not want me in politics
because he was
concerned that I might have affairs with my colleagues. I secretly
joined a
political party without his permission. When he discovered, he beat me
badly.
After much pleading, he eventually allowed me to join again, although
with a
serious condition. I agreed to his condition that, “if I see you
having
affairs, I will send you out of this house.” This means that I
would be denied
access to our children and whatever assets we have both acquired. In
spite of
this condition, I am still restricted in my everyday life and this
prevents me
from participating effectively in political activities.
Religion
and gender roles:
All the participants indicated that their religious environment play a
significant role in shaping women’s sexual behaviour to fit with
men’s
preferences. A few women expressed strong desire for a change. A HSW
stated:
They
preach in mosques and churches that we should submit
to our husbands. They expect us to put up with unpleasant situations.
This is
unfair and I think we should be able to insist on our rights.
However,
many proposed a less aggressive alternative, as
a HSW said, ‘in Africa we are very religious, so I will keep
praying to God
that I want my husband to change but I cannot insist on condom
use.’ For many
women in a similar context, acceptance of male dominance, as their
religions
and tradition stipulate, is necessary to achieve a degree of meaningful
life
(Jewkes and Morrell, 2012). Comments from some of the men corroborate
the
indications that religious ideologies contribute to why women are
vulnerable to
HIV infection. A LSM said:
In
support of SDM, this finding indicates that HIV
programmes need to recognise the roles religious environments play in
shaping
women’s sexual behaviour. What is more, some of the women
indicated that they
had internalized such a religious ideology as they expressed the belief
that
gender equality in sexual relationships is a utopian concept,
‘God did not make
men and women equal,’ a HSW said. She added:
The
acceptance and internalization of such gender stereotype
would mean that many women in this society are unlikely to be willing
to defend
their rights to exercise control over their sex lives. Thus, HIV
programmes
targeting this society must be designed to recognise that women are
sometimes
both victims and active promoters of the gender inequality and other
cultural
practices that disadvantage women (Jewkes and Morrell, 2012; O'Connor
and
Drury, 1998; Shneider, 2004).
Culture
of silence about sex: This is a widely acceptable cultural
phenomenon
among the Yoruba people, which seems to weaken the prescriptions of BM
on HIV
prevention. BM is sympathetic to public discussions about sex and
condom use in
the form of health promotion. On the contrary, as influenced by the
culture of
silence about sex, most of the participants considered open discussions
about
sex offensive, immoral, and tantamount to fostering promiscuity and
reckless
sexual behaviour, especially among young people. A HSW said that,
The
participants did not only indicate that there was a
widespread belief that condoms equates with promiscuity or
unfaithfulness, they
also suggested that the possession of or public discussions about
condoms
attract social stigma. In view of that, they acknowledged that this
factor
contributes to why people avoid using condoms. According to a HSM,
‘I would
feel ashamed to go and buy condoms, even if I intended to use them with
my
wife.’ To reduce the stigma associated with the possession of
condoms, another
HSM stated that local names have been created for them, ‘fere
daddy’
(daddy’s balloon), ‘agbeojo (rain coat/umbrella),
and ‘kini yen’
(that thing). Yet there is widespread antipathy to explicit
communication about
sex and condoms because of the perception that it undermines their
tradition,
moral values, and religious principles. Literature has shown that women
and
girls are more disadvantaged by this culture of silence about sex (WHO,
2009).
Conformity to societal expectations means that they are more likely to
be
ignorant of basic information about sexual and reproductive health.
Therefore,
to achieve effective communications about HIV/AIDS programmes needs to
be more
sensitive to social and cultural elements.
Desire
for fertility:
This is another major factor, which contributes to HIV incidence among
Yoruba
women. In many African societies, having a biological child is an
important
phase of life. People regard this as a status symbol with high social
ranking
(Doyal and Anderson, 2005). To demonstrate their fecundity, in
conformity to societal
expectations, women of reproductive age unavoidably have to engage in
unprotected sex. As one the LSW stated, ‘It would be difficult
for me to insist
on condom use because I am trying to have a child.’ This
woman’s desire for
fertility means avoidance of condom use, which in turn, could increase
her
vulnerability to HIV infection, especially if her partner engages in
high-risk
behaviour (United Nations Secretariat, 2002). As an example of how
factors
outside women’s control influence their sexual behaviour, this
finding does not
support the assumptions of BM. Considering the findings above, it begs
the
question whether Yoruba women have the capacity to make free health
choices
about HIV prevention even though there are social and structural
barriers. This
statement is explored further in the following section.
Behavioural
determinants of HIV/AIDS
Discussions
in this section suggests that it is not
always that case Yoruba women are not capable of making free choices
about
their sexual behaviour, thus weakening the assumptions of SDM. In
addition, the
participants indicated the roles of biology in shaping sexual behaviour.
Condoms
avoidance to maximize sexual
satisfaction:
A study has indicated that consistent use of
condoms could deliver 80 percent reduction in HIV incidence (Wilkinson,
2002),
which means this is still the most effective approach to preventing
sexually
transmittable infection. However, ample evidence exists that many
people, women
and men, avoid using condoms because of the perception that they reduce
sexual
satisfaction (Higgins et al., 2010). In support of BM, findings
from
this study have also shown that avoidance of condoms is a calculated
choice
that many Yoruba people make to achieve undiminished sexual
satisfaction.
Discussing this issue, a LSM said that,
In
suggesting that his partner is an active player in
deciding whether to use condoms or not, this man’s comment
contrast with the
vulnerability perspective of SDM, which suggests that women’s
inability to
negotiate condom use is primarily a result of inequality in gender
power
relations (Higgins et al., 2010). Corroborating the evidence
that women
sometimes make free choices regarding condom use, a LSW said to me
that,
‘condoms have holes in them, therefore I think there is no point
using them if
they cannot guarantee a full protection.’ In this case, it is
reasonable to
argue, in support of BM, that access to accurate information about
condoms and
HIV prevention will encourage such a woman to engage in risk-reducing
behaviour.
Fear
of unwanted pregnancy:
More evidence emerged of how some of the women exercise control over
their sex
lives as a LSW stated that,
In this context, the use of condom seems to be synonymous
to birth control rather than a means to prevent sexually transmittable
infections. Nonetheless, it is important to note that this woman
indicated that
she was able to make free choices about her sex life. As such, her
comment
strengthens BM by implying that women sometimes play active roles in
deciding
whether to use condoms or not. Hence, it can be a difficult task to
ascertain
when structure or agency is dominant in shaping women’s sexual
health
behaviour. Besides behavioural and social determinants, the
participants
indicated that biology also play significant roles in shaping sexual
behaviour.
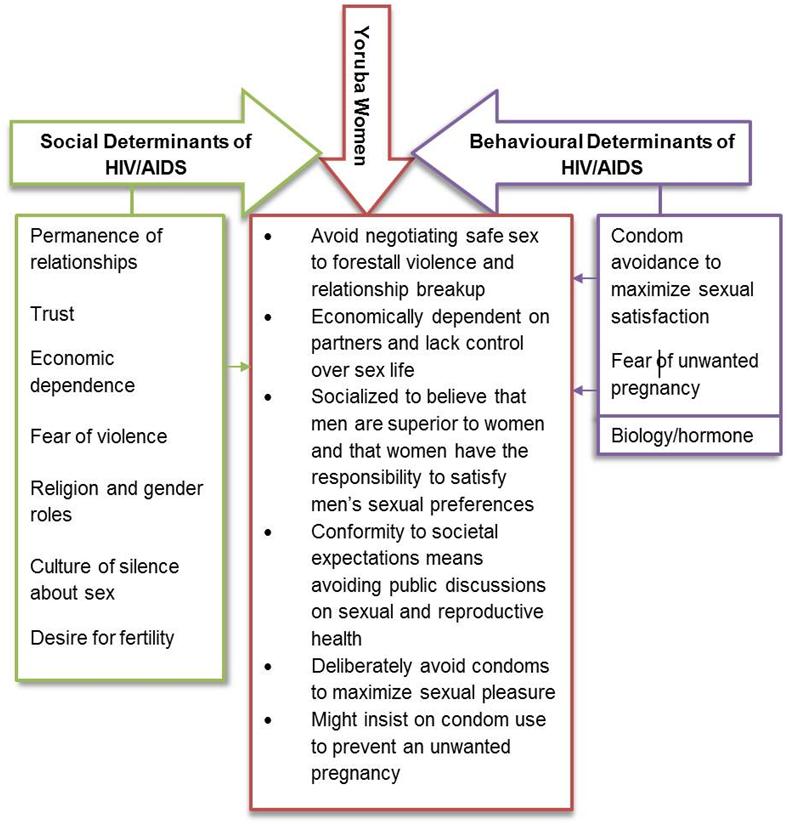
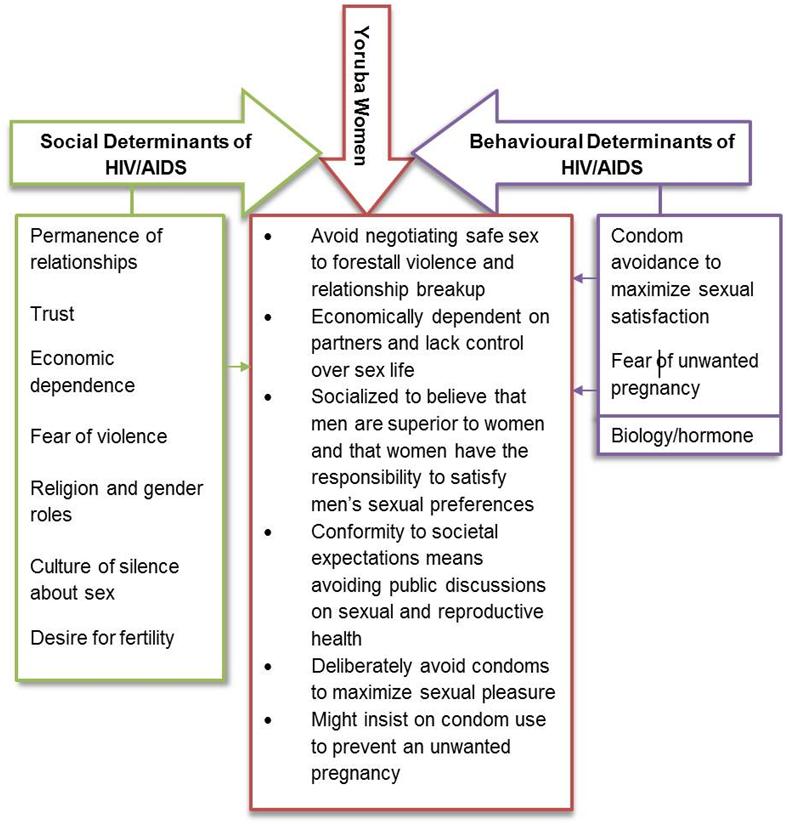
Figure
1: A Summary of the Findings
Human
biology and sex behaviour:
Some of the participants, men in particular, indicated that condom use
is not a
decision that they always have control over. According to a HSM,
‘the momentary
pressure experienced before a sexual intercourse does not give room for
negotiating condom use.’ Many of the participants intended to
suggest that
because of their biology, they often behave in an instinctive manner,
with
little or no control over their actions when sexually aroused. However,
because
this is a subjective experience, which varies between individuals, it
would be
difficult to measure the degree to which it is true that hormonal
pressure
limits individual’s ability to use condoms.
Old
age is another biological factor that some of the men
highlighted as a limitation in prevention HIV. Without a clinical
history of
erectile disorder, a 61 year old LSM said:
It
is normal for older men to have trouble with
erections. Without a sustainable erection, how could I use a condom?
The last
time I tried using one, I felt embarrassed as my partner watched me
struggling.
Before I could put it on, my thing [penis] became soft.
As
some of the participants have shown that condoms might
not be the appropriate method for HIV prevention among older men,
consequently,
it might be difficult for women to negotiate condom use with such men.
Conclusion
In
reference to the United Nations Millennium Development
Goals, there are worldwide acknowledgements that women in SSA need to
be
empowered to reduce their susceptibility to HIV/AIDS (United Nations,
2007).
The question remains, how could they be empowered? As illustrated in
this
article, the experiences of the Yoruba women have exposed the
limitations of
both BM and SDM, which means these models are not exclusively accurate
in
prescribing how to empower such women to prevent HIV/AIDS. Clearly,
access to
information and education is not enough. Despite having at least a
basic
knowledge of HIV prevention, most of the participants indicated that
their
sexual behaviour is inconsistent with this knowledge. Thus, it would be
inadequate to limit programmes to behavioural interventions. Likewise,
because
access to economic power and higher education did not seem to make a
big
difference among the high status women in negotiating safe sex with
partners,
the SDM is weakened.
Given
these limitations, it has been suggested that a
combination prevention model is a much better alternative (UNAIDS,
2010). This
approach requires a simultaneous use of complementary behavioural,
biomedical,
and social prevention strategies, while focusing on different levels of
interventions (individuals and groups), to address the specific but
diverse
needs of the populations at risk. In the context of Yoruba communities,
more
needs to be done in terms of providing access to accurate information
about HIV
prevention. However, because of poor infrastructure, rather than
concentrating
on conventional mass media programmes, more support should be given to
community workers to provide life skills tailored to the needs of
individual
groups in their communities. In addition, women need to be empowered,
but must
be supported to define clearly what empowerment means to them. Such
empowerment
should take into account factors such as: access to life chances
(education and
employment); participation in domestic and public decision making
process;
control over family assets; freedom of movement and association; legal
protection against injustice, discrimination, and harmful traditional
practices; and guaranteed access to state social
securities.
Lastly,
there is a case for saying that SDM and BM, as
they are currently, do not complement each other because they have
different
epistemological positions and commit to different policies. Hence,
further
research is required to understand how they could be developed to
complement
each other and the extent to which prominence should be given to either
in a
specific context.
Appendix
Distribution of Respondents
| Groups | IDIs | FGDs |
| Low status women | 6 | 1 (11 women) |
| High status women | 6 | 1 (11 women) |
| Low status men | 5 | 1 (10 men) |
| High status men | 5 | 1 (10 men) |
| Local HIV/AIDS agencies | 7 (4 women, 3 men) | None |
| HIV positive participants | 10 (6 women, 4 men) | 2 (10 women, 10 men) |
| Pilot studies | None | 2 (10 women in each) |
| Total | 39 (22 women, 17 men) | 8 (52 women, 30 men) |
Acknowledgements
The
author thanks Professor Mick Carpenter and Dr Phil
Mizen for their invaluable feedback on my PhD thesis, from which this
article
was drawn.
References
Amaro,
H. (2000), ‘On the margin: Power and women's HIV
risk reduction strategies’, Sex Roles,42 (7-8), pp.723-49.
Amaro,
H., A. Raj and E. Reed (2001), ‘Women’s sexual
health: the need for feminist analyses in public health in the decade
of
behaviour’, Psychology of Women Quarterly, 25 (4),
pp.324–34.
Argemi,
X., S. Dara, S. You, J. Mattei, C. Courpotin, B. Simon,
Y. Hansmann, D. Christmann and N. Lefebvre (2012), ‘Impact
of malnutrition
and social determinants on survival of HIV-infected adults starting
antiretroviral therapy in resource-limited settings’, AIDS,
26 (9),
pp.1161–166,.
Bambra,
C., M. Gibson, A. Sowden, K. Wright, M. Whitehead
and M. Petticrew (2010), ‘Tackling the wider social determinants
of health and
health inequalities: Evidence from systematic reviews’, Journal
of
Epidemiology and Community Health, 64, pp.284-91.
Berkman,
L. and Kawachi, I. (2000), ‘A Historical
Framework for Social Epidemiology’, in Berkman, L. and Kawachi,
I. (eds), Social
epidemiology. New York: Oxford University Press, pp.3-12.
Blas,
E., L. Gilson, M. Kelly, R. Labonté, J. Lapitan, C.
Muntaner, P. Ostlin, J. Popay, R. Sadana, G. Sen, T.
Schrecker
and Z. Vaghri (2008), ‘Addressing social determinants of
health
inequities: What can the state and civil society do?’, Lancet,372
(9650),pp.1684–9.
Blumberg,
S. (2000), ‘Guarding against threatening HIV
prevention messages: An information processing model’, Health
Education
&Behavior,27 (6), pp.780–95.
Bowleg,
L., F. Belgrave and C. Reisen (2000), ‘Gender
roles, power strategies, and precautionary sexual self-efficacy:
Implications
for Black and Latina women’s HIV/AIDS protective
behaviours’, Sex Role,42
(7-8),pp.613–35.
Commission
on Social Determinants of Health (2008), Closing
the gap in a generation: Health equity through action on the social
determinants of health, http://whqlibdoc.who.int/publications/2008/9789241563703_eng.pdf,
accessed 10 September 2009.
Dane,F.
(1990), Research
Methods,California:Brooks/ColePublishing.
Doyal,
L. and J. Anderson (2005), ‘My fear is to fall in love
again...' How HIV-positive African women survive in London’. Social
Science
and Medicine, 60 (8), pp.1729-738.
Economic
and Social Research Council (2012), ESRC
Framework for Research Ethics (FRE) 2010 Updated September 2012, http://www.esrc.ac.uk/_images/Framework-for-Research-Ethics_tcm8-4586.pdf
, accessed 15 January 2013.
Fetterman,
D. (1998), Ethnography: Step by Step, Applied
Social Research Methods,Vol. 17, Thousand Oaks, California:
Sage
Publications.
Fishbein,
M. (2000), ‘The role of theory in HIV
prevention’, AIDS Care, 12 (3), pp.273-78 https://wiki.umn.edu/pub/EWB/UgandaCommunityHealth/The_role_of_theory_in_HIV_prevention.pdf,
accessed 14 May 2011.
Fishbein,
M. (2008), ‘A Reasoned Action Approach to
Health Promotion’, Medical Decision Making, 28 (6),
pp.834-44.
Gillespie,
S., S. Kadiyala and R. Greener (2007), ‘Is
poverty or wealth driving HIV transmission?’,AIDS, 21
(issue supplement
7), S5–S16.
Glanz,
K., B. Rimer and F. Lewis (2002), Health
Behaviour and Health Education: Theory, Research, and Practice.
California:
Jossey-Bass Publishers (originally published by the same publisher in
1990).
Gupta,
G. (2002), ‘How men's power over women fuels the
HIV epidemic’, British Medical Journal, 324 (7331),
183–84.
Gupta,
G., J. Parkhurst, J. Ogden, P. Aggleton and A.
Mahal (2008), ‘Structural approaches to HIV prevention’, Lancet,
372
(9640), 764-75.
Higgins,
J., S. Hoffman and S. Dworkin (2010),
‘Rethinking Gender, Heterosexual Men, and Women’s
Vulnerability to HIV/AIDS’, American
Journal of Public Health,100 (3), pp.435-45.
Jewkes,
R., K. Dunkle, M. Nduna and N. Shai
(2010), ‘Intimate
partner violence, relationship power inequity,
and incidence of HIV infection in young women in South Africa: A cohort
study’,
Lancet,376 (9734), pp.41–48.
Jewkes,
R. and R. Morrell (2012), ‘Sexuality and the
limits of agency among South African teenage women: Theorising
femininities and
their connections to HIV risk practices’, Social Science and
Medicine,
74 (11), pp.1729-737.
Joint
United Nations Programme on HIV/AIDS (2010), Combination
HIV Prevention: Tailoring and Coordinating Biomedical, Behavioural and
Structural Strategies to Reduce New HIV Infections: A UNAIDS Discussion
Paper.
http://www.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2011/20111110_JC2007_Combination_Prevention_paper_en.pdf,
accessed 20 March 2011
Joint
United Nations Programme on HIV/AIDS(2012), Report on the Global AIDS Epidemic,http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf,
accessed 16 May 2013.
Kim,
J., P. Pronyk, T. Barnett and C. Watts (2008),
‘Exploring the role of economic empowerment in HIV
prevention’, AIDS, 22
(issue supplement 4), S57–S71.
Lee,
R. (1999), Doing research on sensitive topics,
London: Sage publications.
Lisk,
F. (2010), ‘Global Institutions and the HIV/AIDS
Epidemic: Responding to an international crisis’, London:
Routledge.
Maman,
S., J. Mbwambo, M. Hogan, G. Kilonzo, J. Campbell
and M. Sweat (2002), ‘HIV-1 Positive Women Report More Lifetime
Experience with
Violence: Findings from a Voluntary HIV-1 Counseling and Testing Clinic
in
Dares Salaam, Tanzania’, American Journal of Public Health,92
(8),
pp.1331-337.
Marmot,
M., S. Friel, R. Bell, T. Houweling and S. Taylor
(2008), ‘Closing the gap in a generation: Health equity through
action on the
social determinants of health’, Lancet, 372 (9650),
pp.1661–669.
Mongkuo,
M., R. Mushi and R. Thomas (2010), ‘Perception
of HIV/AIDS and socio-cognitive determinants of safe sex practices
among
college students attending a historically black college and university
in the
United States of America’, Journal of AIDS and HIV Research,
2 (3),
32-47.
Moulin,
A. (2008), The World Health Organization and
the Social Determinants of Health: Assessing Theory, Policy and
Practice, http://www.ucl.ac.uk/histmed/downloads/social_determinants/comments/wellcomewhocairo.pdf,
accessed 12 October 2010.
Murphy,
E., M. Greene, A. Mihailovic and P. Olupot-Olupot
(2006), ‘Was the “ABC” Approach (Abstinence, Being
Faithful, Using Condoms)
Responsible for Uganda's Decline in HIV?’, PLOS Medicine,
3 (9),
e379, doi:10.1371/journal.pmed.0030379, http://www.plosmedicine.org/article/info:doi/10.1371/journal.pmed.0030379,
accessed 24 June 2010.
Navarro,
V. (2009), ‘What we mean by social determinants
of health’, Global Health Promotion, 16 (1), pp.5-16.
National
Population Commission and ICF Macro, (2009), Nigeria
Demographic and Health Survey 2008: Key Findings.
Calverton,
Maryland: National Population Commission and ICF Macro, http://www.measuredhs.com/pubs/pdf/SR173/SR173.pdf,
accessed 15 July 2012.
O'Connor,
F. and B. Drury (1998), The Female Face in
Patriarchy: Oppression as Culture, Michigan: State University
Press.
Power,
R. (1998), ‘The Role of Qualitative
Research in HIV/AIDS’, AIDS, 12 (7), 687-95,
Prochaska,
J., S. Butterworth, C. Redding, V. Burden, N.
Perrin, M. Leo, M. Flaherty-Robb and J. Prochaska (2008),
‘Initial efficacy of
MI, TTM tailoring and HRI’s with multiple behaviors for employee
health
promotion’, Preventive Medicine, 46 (3), pp.226-31.
Rawls,
J. (1971), A Theory of Justice, Cambridge,
Massachusetts: Harvard University Press.
Rimer,
B. and K. Glanz (2005), Theory at a Glance: A
Guide for Health Promotion Practice,National Institute of Health
(first
edition published in 1995) http://www.cancer.gov/cancertopics/cancerlibrary/theory.pdf,
accessed 04 July 2010.
Rosenstock,
I., V. Strecher and M. Becker (1994), ‘The
Health Belief Model and HIV risk behavior change’, in DiClemente,
R. and
Peterson, J. (eds.), Preventing AIDS: Theories and methods of
behavioural
interventions, New York: Plenum Press, pp.5-24.
Rubin,
H. and I. Rubin (2012), Qualitative
Interviewing: The Art of Hearing Data, Los Angeles: Sage
Publications
(originally published by the same publisher in 1995).
Ruger,
J. (2004), ‘Ethics of the social determinants of
health’, Lancet, 364, 092–097.
Sen,
A. (2001), Development as Freedom, Oxford:
Oxford University Press.
Shelton,
J., M. Cassell and J. Adetunji (2005), ‘Is
poverty or wealth at the root of HIV?’,Lancet, 366 (9491),
pp.1057-058.
Shneider,
D. (2004), The Psychology of Stereotyping,
New York: The Guilford Press.
Skinner,
B.F. (1938), Thebehavior of organisms: an
experimental analysis, New York: Appleton-Century-Crofts.
Sobo,
E. (1995), Choosing Unsafe Sex: AIDS Risk Denial
among Disadvantaged Women, Philadelphia, PA: University of
Pennsylvania
Press.
Stevens,
P. (2009), ‘Bias in WHO report on the social
determinants of health’, Lancet, 373 (9660), 298, doi:
10.1016/S0140-6736(09)60091-X.
Stewart,
D., P. Shamdasani and D. Rook (2007), Focus
Groups: Theory and practice, applied social research methods
series vol.
20, Thousand Oaks, California: Sage Publications Inc.
United
Nations (2007), Africa and the Millennium
Development Goals 2007 update, New York: United Nations, http://www.un.org/millenniumgoals/docs/MDGafrica07.pdf,
accessed 16 May 2011.
United
Nations General Assembly Special Session (2010), Country
Progress Report: Nigeria. http://data.unaids.org/pub/Report/2010/nigeria_2010_country_progress_report_en.pdf
access 23 July 2011.
United
Nations Secretariat (2002), HIV/AIDS and
Fertility in Sub-Saharan Africa: A Review of the Research Literature.Esa/P/Wp.174.
http://www.un.org/esa/population/publications/fertilitysection/HIVAIDSPaperFertSect.pdf,
accessed 02 February 2011.
Watters,
J. and P. Biernacki (1989), ‘Targeted sampling: Options
for the study of hidden populations, Social Problems, 36 (4),
pp.416-30.
Welsh,
E. (2002), ‘Dealing with Data: Using NVivo in the
Qualitative Data Analysis Process. Forum: Qualitative Social
Research’,
3(2)
http://nbn-resolving.de/urn:nbn:de:0114-fqs0202260,
accessed 10 January 2012.
Wiles,
R., G. Crow, S. Heath and V. Charles (2006), ‘Anonymity
and Confidentiality’, Paper presented at the ESRC Research
Methods
Festival, University of Oxford, July 2006. http://www.ccsr.ac.uk/methods/festival/programme/aac/documents/anonandconfpaperRMF06.pdf,
accessed 11 June 2011.
Wilkinson,
D. (2002), Condom effectiveness in reducing
heterosexual HIV transmission: RHL commentary, The WHO Reproductive
Health
Library, Geneva: World Health Organization, http://apps.who.int/rhl/hiv_aids/dwcom/en/,
accessed 12 February 2011.
Wilkinson,
R. and M. Marmot (eds.) (2003), Social
determinants of health: The solid facts,World Health Organization, http://www.euro.who.int/__data/assets/pdf_file/0005/98438/e81384.pdf,
accessed 21 May 2011.
World
Health Organization (2009), Gender inequalities
and HIV, http://www.who.int/gender/hiv_aids/en/
accessed 21 July 2011.